ME / Chronic Fatigue Syndrome News
Here I share Chronic Fatigue Syndrome news to communicate information about the chronic illness CFS (also known as ME - Myalgic Encephalomyelitis).
The article below may also be of interest to those with other auto-immune illnesses who are seeking information on research findings and the science of the illness with which they live.
Relevant chronic illnesses include CFIDs, SEID, Fibromyalgia, Post Viral Fatigue and Long Covid aka Covid long haul.
2023 research includes a finding on how the science confirms an overlap between Long Covid and Myalgic Encephalomyelitis.
Or click here to CHOOSE FROM
A RANGE OF personalizable cards and gifts.
The healing-themed gifts are designed by myself, Katherine, the author of
this website HealingCFSME.com
Proceeds go towards the cost of the website. Thank you. Enjoy!
If you wish to add your own ME or Chronic Fatigue Syndrome news please feel free to share your wisdom and experience on the healing forum.
Below: This is me enjoying a change of scene on a local trip to Avebury, UK. I was well enough to go but not well enough to walk when I got there.
Contents for Chronic Fatigue Syndrome News
Much of the research is organised by year. The years are in reverse order as I add the latest CFS research nearer the top of the page.
I have also collated some research into specific subjects. Click to see the specific subjects of research.
Click on the above 2024 link for this Chronic Fatigue News
- The LOCOME – long Covid and Myalgic Encephalomyelitis diagnostics and stratification project.
Click for this Chronic Fatigue News and more ....
- phD student chooses ME/CFS research
- Excess WASF3 protein in CFS patients affects energy production
- ME/CFS is finally on the syllabus when training UK doctors
- A way found to distinguish between myalgic encephalomyelitis, fibromyalgia and other comorbidities
- Micro-clotting observed in both Long Covid and ME patients
- Two-years follow-up of symptoms and return to work in Complex Post-COVID-19 Patients
2021 Chronic Fatigue News
- Chronic Fatigue Syndrome (Cfs) And Fibromyalgia Are Vascular Disease.
- Genetics
- Abilify - the drug that is helping Whitney Dafoe at the time of writing
2020 Chronic Fatigue News
- June 2020. RESEARCH. Request for 20,000 volunteers to send in saliva sample. PLEASE SHARE.
DecodeME DNA study announcement - November 2020 Canadian Researchers develop a blood biomarker to identify ME/CFS patients.
- Mitochondrial dysfunction in people with ME/CFS. Paul Fisher, Australia.
- Stanford University research: A chronic fatigue syndrome blood test gives 100% accuracy
- Griffiths University research: The drug nifedipine helps to reveal impaired pathology in CFS/ME
- Problems with brain functioning in those with the chronic illness CFS/ME
2018 Chronic Fatigue News
Apologies but I haven't managed to keep up with much Chronic Fatigue Syndrome / ME research in 2018. Here are a few items!
- Chronic fatigue syndrome test shows 84 percent accuracy
- Brain inflammation found in patients with ME/CFS - This link goes through to a separate page of research into Chronic Fatigue Syndrome news about research into the brain.
- Overactivity of the immune system 'may trigger ME-like symptoms'
- Interview with Doctor David M. Systrom, MD
2017 Chronic Fatigue News
- Impaired cellular bio energetics in patients
with Myalgic Encephalomyelitis
- Cytokines in the blood match symptom severity in Chronic Fatigue Syndrome/ ME
- The UK government comment on the absence of an effective policy for the treatment of Myalgic Encephalomyelitis
- USA. Correlation shown between gut disturbance and severity of CFS/ME symptoms
- Canada. Researchers identify differences across the genome in CFS patients.
- National Institute of Health (NIH) commits to find medical answers to help those with Chronic Fatigue Syndrome.
- Gene expression demonstrates the severity of illness in people with CFS/ME.
- Chronic Fatigue Syndrome news - the illness is linked to a faulty cell receptor in immune cells.
Chronic Fatigue Syndrome News for 2013-2016
Click here for Chronic Fatigue Syndrome News for 2013-2016, or click on the year related to the CFS research of interest.
Any problem with the link, let me know!
The following years are now listed in chronological order, as I was getting confused!
But are still currently in reverse order when you click through to the page. Sorry!
The relaxation response can improve mitochondrial function
- Chronic mycoplasma infection found in 50% of CFS patients
- Higher levels of cytokines in those with CFS/ME in the first 3 years
- USA initiative to rename the illness Chronic Fatigue Syndrome to bring greater recognition of this serious chronic illness.
- Amino acid research on people with Chronic Fatigue Syndrome.
Energy metabolism in chronic fatigue syndrome patients. Is the body acting as though it is starving? - Japanese research finds a test to differentiate between normal fatigue and pathological fatigue.
- Possible blood test for Chronic Fatigue Syndrome - Are people with CFS in hibernation?!
Chronic Fatigue Syndrome news prior to 2012
Click through for the following Chronic Fatigue Syndrome news prior to 2012 and for a list of CFS blogs by other people
- CFS Research on difficulty standing still
- Blog on Multiple Sclerosis
- Research into how to overcome fatigue
- Lyme Disease - an illness with similar symptoms to CFS / Myalgic Encephalomyelitis
- CFS/ME is taken seriously by authorities - patients are not allowed to donate blood
- A Film/DVD/ Movie about CFS/ME
Research divided into specific topics
Research: Chronic Fatigue Syndrome and exercise
- A CFS article on Doctor's quotes on the harms associated with ME/CFS and exercise.
- A CFS article sharing research into why a person with ME/CFS feels worse after exercise. Useful information for benefit claims, or explaining to loved ones or health professionals.
Research: The brain and Myalgic Encephalomyelitis
Click through for the following two articles on research into the brain and Myalgic Encephalomyelitis
- Brain abnormalities identified in CFS/ME patients, Stanford study
- Brain abnormalities in patients with CFS (Myalgic Encephalomyelitis) - PET scans
Research into a drug for Myalgic Encephalomyelitis
The search for a drug for Myalgic Encephalomyelitis /CFS - what has been researched?
Click on the link above for all of the following CFS news:
- 2017. Can anti-inflammatory drugs help people with CFS?
- 2011. Rituximab - a possible cure for CFS/ME? Based on a treatment for cancer.
- 2013. Cancer treatment may be a treatment for CFS - Low dose naltrexone (LDN)
- 2013. Can antidepressants relieve CFS symptoms? - Research on amitriptaline for CFS pain relief and help with sleep
Chronic Fatigue Syndrome Research and News
2025 back to 2017 is listed below
Chronic Fatigue Syndrome News in 2025
Published when: 2025
Published where. A study published in the journal EMBO Molecular Medicine.
Sample size: The research was based on data from the UK Biobank, drawing on health data and biological samples of 500,000 UK participants.
Method: Researchers compared blood samples from 1,455 ME patients with more than 131,000 healthy people.
Confirmation. The findings were compared and replicated in data from a group of American patients and healthy controls.
Result: The identification of differences in concentrations of cell counts and molecules between the studied group and the healthy control group.
The differences in samples for the ME patients were related to the following:
* chronic inflammation
* insulin resistance
* liver dysfunction.
Researchers found 116 “biomarkers” for ME in the blood of men and women with the condition.
Names associated with the research. Prof Chris Ponting, Edinburgh University’s Institute of genetics and Cancer. Dr Sjoerd Beentjes, of the Edinburgh University School of mathematics:
Chronic Fatigue Syndrome News in 2024
ME/ CFS News Announcement April 2024
Action for ME, PrecisionLife and the MRC human genetics unit at the University of Edinburgh have been awarded a 622,000 grant by innovate U.K.’s advancing precision medicine program to improve diagnosis and treatment for the millions of people affected by MEE/CFS and long Covid.
The project is called LOCOME – long Covid and Myalgic Encephalomyelitis diagnostics and stratification project.
PrecisionLife has previously analysed a group of patients from long Covid and DecodeME datasets.
This project will extend their analyses and go into greater depth.
Precision medicine recognises that people with a particular disease may share a diagnosis but have different causes (and respond to different treatments. It sets out to identify the unique biological cause of the disease.
“ME/CFS and long Covid come at a high cost – to the people living with these conditions, the economy, and the NHS – yet we know less about the molecular causes and how to treat them effectively than we do about many rare and less disabling diseases,”
“By injecting badly needed robust genetic evidence into these research fields, and by improving the wider perception of research in these areas, we hope to encourage skilled investigators to apply their cross disciplinary expertise to address future challenges in ME/CFS and long Covid research.”
Prof Chris Ponting, University of Edinburgh
Click here for more helpful quotes by doctors about ME/CFS, Myalgic Encephalomyelitis
This information is shared with grateful thanks to the Interaction magazine, the magazine of the UK ME Action charity
Chronic Fatigue Syndrome News in 2023
Useful disability tips
For those with hidden disabilities such as low mobility.
You can buy a sunflower lanyard (hdsunflower.com). This alerts staff, for
example at an airport, that you have mobility problems.
These are available in many countries.
phD student chooses ME/CFS research
In 1984 there was an outbreak of what was later called ME at Lake Tahoe Nevada,
A doctor, Dr Peterson made a commitment to document and sample this community and has done so from that time to the present day.
In 2023, his work has been studied by Audrey Ryback in the final year
of her PhD at the University of Edinburgh , work funded by the Wellcome
foundation.
Her research looked into the role of the immune system in ME/CFS.
Audrey is a biomedical researcher.
Audrey hopes to build a career in research to work on blood biomarkers for a ME/CFS.
She regards research into ME/CFS as an important and exciting research field.
Excess WASF3 protein in CFS patients affects energy production
When: August 2023
Who: Hwang along with NIH researcher Brian Walitt
Where: a laboratory at the National Heart, Lung and Blood Institute. Bethesda, Maryland, USA
Discovery:
Inside the mitochondria skin cells from a patient with fatigue produce an excess
of a protein called WASF3.
Like a stick jammed into bicycle spokes, the overabundant protein WASF3 was gumming up the gears of energy production.
Sample size small: 9 to 14 patients
For more information:
https://www.pnas.org/doi/10.1073/pnas.2302738120
Washington post article here:
https://www.washingtonpost.com/health/2023/09/17/fatigue-cfs-longcovid-mitochondria/
ME/CFS is now! on the syllabus when training UK doctors
Up until 2023 UK doctors have often not received education about Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
In research by Muirhead 41% of universities didn’t teach medical students about this chronic illness.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8230290/
From now on the Medical Licensing Assessment Map provided by the UK General Medical Council will include the illness within the curriculum.
Way to distinguish between myalgic encephalomyelitis, fibromyalgia and other comorbidities
Date Published: 2nd February 2023
Finding: Circulating microRNA expression signatures accurately distinguish between myalgic encephalomyelitis, fibromyalgia and other comorbidities such as MCAS and POTS
Where: Researchers from the University of Montreal and the CHU Sainte-Justine (to check)
Team leader: Professor Alain Moreau
What? The identification of a blood biomarker to identify patients with ME and CFS.
MicroRNA are a family of molecules that help cells to control the amounts and kinds of protein they make. Moreau uses micro-RNA to identify differences in genetics both between different Myalgic Encephalomyelitis/CFS patients and between those with ME/CFS and those with illnesses which are similar.
Published where? journal of Scientific Reports
number of participants: 140
More information here: https://www.nature.com/articles/s41598-023-28955-9
Ongoing research: Aim - to determine a single blood test to indicate ME/CFS.
With thanks to the newsletter of the 25% ME Group in the UK (Scotland)
Micro-clotting in both Long Covid and ME patients
Where: South Africa and UK joint research
South Africa - Prof Pretorius, University of Stellenbosch
UK - Prof Kell, Liverpool University
What: Research showing biological similarities in those with Long Covid and ME Myalgic Encephalomyelitis
Results: Blood samples from people with Long Covid show micro clotting.
Blood samples from people with ME patients showed the same.
These clots cause problems in the vascular system. They clog up smaller blood vessels and deprive them of oxygen.
Oxygen deprivation and the affect on brain, muscles and other organs could explain the diverse symptoms in ME and long covid
Two-Years Follow-Up of Symptoms and Return to Work in Complex Post-COVID-19 Patients
Conclusion: only 9% recovery
More information here: https://www.mdpi.com/2077-0383/12/3/741
Chronic Fatigue Syndrome News in 2021
Chronic Fatigue Syndrome (Cfs) And Fibromyalgia Are Vascular Disease
When: October 2021
https://www.researchgate.net/publication/355081782_CHRONIC_FATIGUE_SYNDROME_CFS_AND_FIBROMYALGIA_ARE_VASCULAR_DISEASE
Who and where:
Gustavo Aguirre Chang, National University of San Marcos
Aurora Natividad Trujillo Figueredo, SIGESA
Please copy and paste the link to find out more.
Drug treatment for CFS/ME - Abilify helps some
Abilify is a drug that is helping Whitney Dafoe with cognitive function at the time of writing.
There is an excellent article on the website Health Rising.
https://www.healthrising.org/blog/2020/10/03/celebrating-whitney-dafoe-awakening-37th-birthday
Abilify is usually used for conditions like bi-polar or schizophrenia and at a much higher dose.
The comments are also worth reading.
They suggest that for some Abilify is a solution that lasts for months rather than longterm.
Some find if they take a break and go back on, it is effective once again.
Even so... to find a treatment that works at all for CFS/ME is a beautiful thing and gives hope.
Chronic Fatigue Syndrome and Genetics
A study reports that having a close relative with the disease may increase your risk of developing Chronic Fatigue Syndrome by 13%.
Who and when: Chu L, Valencia IJ, Garvert DW, Montoya JG. Onset patterns and course of myalgic encephalomyelitis/chronic fatigue syndrome. Front Pediatr. 2019
More on this CFS news here.
https://www.verywellhealth.com/chronic-fatigue-syndrome-genetics-5093946
Chronic Fatigue Syndrome News in 2020
12 November 2020: a blood biomarker
Where: Researchers from the University of Montreal and the CHU Sainte-Justine
Team leader: Professor Alain Moreau
What? The identification of a blood biomarker to identify patients with ME and CFS.
Published where: journal Scientific Reports
More information here: https://www.nature.com/articles/s41598-020-76438-y
June 2020
DecodeME DNA research study announcement
Request for volunteers to send in saliva sample
Funding has been secured for a study to analyse DNA from the
saliva of 20,000 people with ME/CFS.
The aim is to see whether the disease is partly
genetic.
If so, the aim is to help pinpoint the genetic component which causes it.
The study aims to help
bring understanding of the disease and to find treatments.
Press Release: £3.2m funding for DecodeME, largest ever DNA study of ME
Website where you can read FAQs and sign up: http://www.decodeME.org.uk
"We’re
focusing on recruiting from the UK for now and are already well on our
way with early sign-ups.
But we’ll expand to other countries if
necessary,
so if you’re outside the UK, please do sign up now.
You must
be 16 or over to take part. "
Katherine: please do share this as #MEAwareness on your social media channels. Thank you.
Chronic Fatigue Syndrome News in 2019
ME/ Chronic Fatigue Syndrome News, July 2019
Mitochondrial dysfunction in people with ME/CFS
I am indebted to the following information to an article on the wonderful Health Rising website.
You can read more there.
Who:
Paul Fisher, an Australian specialist in neurodegenerative diseases and the mitochondria.
Part of the ME/CFS Discovery Research Network (MDRN), a group of Australian researchers collaborating on ME/CFS. The MDRN was set up in 2018.
Extract:
"ATP production [in the blood of the sample of people with ME/CFS] was normal,
but once Fisher began stressing the energy production systems strange
things began happening.
In particular, Fisher found that Complex V – the
last of the five complexes and arguably the most important – responded
poorly."
"The NIH reports that Complex V Deficiency
can produce a wide variety of symptoms including extreme fatigue, low
muscle tone (hypotonia), increased levels of lactic acid, rapid
breathing, cognitive issues, etc."
"The end result was that the ME/CFS
mitochondria were working harder than ever. They were able to get the
cells’ ATP production up to normal – at rest – but this was not enough
to handle stressful conditions."
He found "that the energy
stressed ME/CFS patients’ cells had moved from breaking down glucose to
breaking down the more ATP-rich fatty acids in order to squeeze out as
much energy as possible."
"Fisher’s intuition [10 years ago] was correct. ME/CFS patients’ mitochondria are having problems producing energy."
ME/ Chronic Fatigue Syndrome News, April 2019
A
chronic fatigue syndrome blood test gives 100% accuracy
Who: Stanford professor of biochemistry and genetics Ron Davis. And Dr Rahim Esfandyarpour.
Where: Stanford University, USA.
Method: The new test measures energy output from immune cells in the blood. The 'nanoelectronic assay' measures how much the energy outputs of these cells change when they are exposed to stress, in this case, modeled by salt. Those with ME/CFS had very reactive blood
Result: A chronic fatigue syndrome blood test from Stanford Uni gave 100% accuracy in a trial of 40 patients
Sample size: 40.
Next steps:
- To see if the result is the same with a larger sample size.
- To test to find a drug that treats Chronic Fatigue Syndrome as revealed by the blood test.
- The test identified those with Chronic Fatigue Syndrome as compared to healthy controls - it shows they have an illness. It now needs to be shown that the blood test result is unique to those with CFS as opposed to including those living with other chronic illnesses.
More information: https://www.dailymail.co.uk/health/article-6973391/A-chronic-fatigue-syndrome-blood-test-finally-prove-condition-exists-study-says.html
On May 21, 2019 the following CFS research was posted on the PNAS website which I believe is more on the same news.
https://www.pnas.org/content/116/21/10250
ME/ Chronic Fatigue Syndrome News, April 2019
The drug nifedipine helps to reveal impaired pathology in CFS/ME
Who: Dr Helene Cabanas and the NCNED research teams
Where: Griffiths University in Australia
Method: "Whole-cell patch-clamp technique was used to measure TRPM3 activity in
isolated NK cells from twelve age- and sex-matched healthy controls and
CFS/ME patients, after activation with pregnenolone sulfate and
[the drug] nifedipine and inhibition with ononetin." Quote with grateful thanks to the Pubmed website - see link below.
Result: Diagnostic marker test developed for ME/CFS, along with a possible drug treatment.
Sample size: 12 or 24 (Katherine - not sure!)
ME/ Chronic Fatigue Syndrome News, March 2019
Problems with brain functioning in those with this chronic illness
The articles shares that "It’s All in Your Head" is true because there are problems with brain functioning in those with this chronic illness.
An interesting article outlining the work of Professor Leonard Jason who himself had or has the illness Chronic Fatigue Syndrome.
Method:Quantitative electroencephalography (qEEG) maps brain waves.
Low-resolution electromagnetic tomography (LORETA)
software investigates the causes of brain dysregulation.
The technology is an upgrade on the MRI.
Conclusion:
Marcie Zinn:
“A normally functioning brain depends on the neurons functioning within a
certain time frame. For patients with ME, the neurons are either
damaged or dead, which causes cognitive impairments because of the
slowed speed and the first part of the processing hasn’t been resolved
before they move on to the next,”
In addition, the research has shown how CFS/ME patients’ everyday waking brain is drowsy because of too many delta waves.
Sample:
Marcie and Mark Zinn have studied the brains of more than 200 patients with ME/CFS
https://depaulmagazine.com/2019/03/14/the-myth-of-its-all-in-your-head/
Chronic Fatigue Syndrome News in 2018
ME/ Chronic Fatigue Syndrome News, December 2018
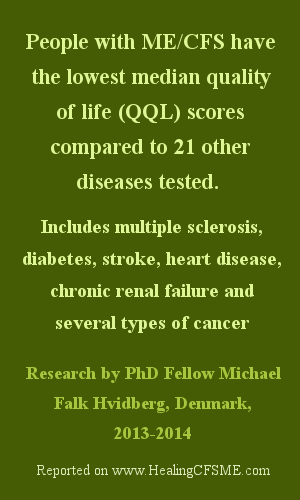
Chronic fatigue syndrome test shows 84 percent accuracy. Animal studies will follow
When published: December 2018
Who: Center for Infection and Immunity (CII). Columbia University's Mailman School of Public Health. New York City, NY. Dr. Dorottya Nagy-Szakal, is one of the authors
What done: Examination of the blood samples of 50 people with ME/CFS. Comparison made with those of 50 age-matched healthy controls
Result: The discovery of 562 metabolites that the people with ME/CFS had in common.
ME/CFS quotes by the scientists behind the study:
Dr Nagy-Szakal:
"This is a strong predictive model that suggests we're getting close to
the point where we'll have lab tests that will allow us to say with a high
level of certainty who has this disorder,".
Dr W. Ian Lipkin:
"We're closing in on understanding how this disease works."
More information: https://www.nature.com/articles/s41598-018-28477-9
ME/ Chronic Fatigue Syndrome News, December 2018
CFS symptoms correlate with over-activity of the immune system
Who? Scientists from the Institute of Psychiatry, Psychology and Neuroscience at King's Colleg, including Dr Alice Russell and Prof Carmine Pariante.
Sample size and type: 55 patients who had hepatitis C.
Intervention: The drug interferon-alpha.
Results: 18 patients developed CFS-like symptoms. In these patients there was a far stronger immune response to the medication. These patients corresponded with those who were measured to have had an overactive immune system prior to treatment .
Statement: "our results are the first step in identifying those at risk and catching the illness in its crucial early stages". Professor Carmine Pariante.
Funding by: Medical Research Council
Published where: the journal Psychoneuroendocrinology
Link to more information:https://www.sciencedirect.com/science/article/pii/S0306453018301963
ME/ Chronic Fatigue Syndrome News, July 2018
Interview with Doctor David M. Systrom, MD
Interview with Doctor David M. Systrom, MD
Works at Brigham and Women's Hospital USA
Reported on youtube by ME/CFS Alert 98
https://youtu.be/FMaKfv8peww
The doctor is angry at his colleagues for mistreatment of ME/CFS patients.
Dr David Systrom's conversation includes a discussion about the connection between the autonomic nervous system (ANS), inflammation and auto immune dysfunction.
Chronic Fatigue Syndrome News in 2017
ME/ Chronic Fatigue Syndrome News, October 2017
Impaired cellular bio energetics in patients with Myalgic Encephalomyelitis
What was the research: A comparison of peripheral blood mononuclear cells.
When was the research published: End of October 2017.
Author of CFS research: Cara Thomas, Newcastle University Ph.D. student (Cara Thomas has lived with ME herself)
Sample size: 52 people with ME and 35 in the control group.
Findings: The cells from those participants living with ME are unable
to meet the energy demands of routine physical tasks. They become exhausted easily when put under
stress.
The suggestion is that chronic fatigue syndrome (CFS) is caused by the body swapping to inefficient methods of energy generation.
Research funded by: Action for ME, Medical Research Council, the ME Association, ME Research UK and the Newcastle Molecular Pathology Node.
Where was this CFS News published:The journal PLOS ONE
Cara Thomas is already planning a follow-up study in which she will test muscle cells in the same way as she has tested blood cells.
Where to read more: https://www.sciencealert.com/chronic-fatigue-syndrome-low-energy-production-in-cells-metabolic-disease
ME/ Chronic Fatigue Syndrome News, 31 July 2017
Cytokines in the blood match symptom severity in Chronic Fatigue Syndrome/ ME
Where:
Stanford University, USA
Who:
Researchers include Jose Montoya, M.D., Mark Davis et al
Results:
The
sample of people with chronic fatigue syndrome showed substantially higher
levels of certain cytokines in their blood.
Changes in levels of these cytokines corresponded with the severity of symptoms of chronic fatigue syndrome.
Cytokines are substances from the immune system.
Conclusion:
There
is a possible link between excess inflammation and Chronic Fatigue Syndrome.
The findings of the research constitute “a solid basis for a diagnostic blood test.” Mark Davis
Where can I read more?
Published online in Proceedings of the National Academy of Sciences
https://med.stanford.edu/news/all-news/2017/07/researchers-id-biomarkers-associated-with-chronic-fatigue-syndrome.html
ME/ Chronic Fatigue Syndrome News, June 2017
The UK government comment on the absence of an effective policy for the treatment of Myalgic Encephalomyelitis
A UK only petition asking for an effective policy for the treatment of Myalgic Encephalomyelitis reached 10,992 signatures.
Selected extracts:
"The Government accepts the World Health Organisation’s classification of CFS/ME as a neurological condition of unknown origin."
"The guideline [The NICE guideline on CFS/ME] recognises there is no one form of treatment to suit every patient and it does not force patients into treatments they do not want. Instead, it emphasises a collaborative relationship between clinician and patient, that treatment and care should take into account personal needs and preferences, and that healthcare professionals should recognise that the person with CFS/ME is in charge of the aims of the treatment programme."
Where can I read more?
Copy and paste this link for the full response:
https://petition.parliament.uk/petitions/190618
ME/ Chronic Fatigue Syndrome News, April 2017
USA. Correlation shown between gut disturbance and severity of CFS/ME symptoms
Just a quick note. There seems to be so much Chronic Fatigue Syndrome news at the moment for me that I can't keep up !
In ME/CFS subgroups, a correlation was shown between the intensity of symptoms including pain and fatigue the presence of distinct bacteria disturbances in the gut.
The trial was made up of 50 ME/CFS cases and 50 healthy controls in the USA.
Who: Dorottya Nagy-Szakal, Brent L. Williams, Nischay Mishra, Xiaoyu Che, Bohyun Lee, Lucinda Bateman, Nancy G. Klimas, Anthony L. Komaroff, Susan Levine, Jose G. Montoya, Daniel L. Peterson, Devi Ramanan, Komal Jain, Meredith L. Eddy, Mady Hornig and W. Ian Lipkin
Read more at:
https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-017-0261-y
ME/ Chronic Fatigue Syndrome News, April 2017
Canada. Researchers identify differences in the genome of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis patients
Where: Canada
Who: Wilfred de Vega, a PhD student, and Associate Professor Patrick McGowan
Published where: The journal of BMC Medical Genomics
Findings: There are many variations in the genome in CFS patients as compared with the control group.These include sites relevant to metabolic processes where the epigenetics are different. (Epigenetics is the study of how genes switch themselves off and on.)
Implication: Researchers can start to develop ways of testing drugs
already in use or develop new therapies to address the differences in the Chronic Fatigue Syndrome population.
Read more at: https://medicalxpress.com/news/2017-04-chronic-fatigue-syndrome.html
ME/ Chronic Fatigue Syndrome News, March 2017
NIH commits to find medical answers to help those with Chronic Fatigue Syndrome
The following is from the website of the National Institutes of Health (NIH) in the USA.
"We recognize and empathize with the suffering experienced by people with ME/CFS and their frustration that so little is known and so little research has been done to find answers. We aim to change that.
The NIH is committed to unraveling the underlying biologic cause(s) of ME/CFS as swiftly as possible, and promoting research that will inform the development of effective strategies for treatment and prevention of this devastating condition."
Click here for the full article.
ME/ Chronic Fatigue Syndrome News, February 2017
A CFS Researcher who has a son with severe Chronic Fatigue Syndrome-ME
Dr Ron Davis works at Stanford university in the genome technology centre.
He has found that gene expression shows that people with CFS/ME are very ill.
Dr Ron's son has severe Myalgic Encephalomyelitis, so he feels great passion and urgency about the research work.
Read more about his work here.
(Another Doctor and researcher with a child with CFS/ME is Dr. Maureen Hanson of Cornell University (New York))
ME/ Chronic Fatigue Syndrome News, February 2017
Chronic Fatigue Syndrome News - faulty cell receptor found in immune cells throughout the body
When was the research published:
February 2017
Who:
T. Nguyen, S. Johnston, L. Clarke, P. Smith, D Staines, S. Marshall‐Gradisnik
Where:
Griffith University's National Centre for Neuroimmunology and Emerging Diseases,
South East Queensland, Australia
Sample size:
40 (25 healthy, 15 with CFS/ME)
Finding:
A faulty cell receptor appears to cause the immune system changes seen in
CFS/ME.
The cell receptor in question is called transient receptor potential melastatin 3 (TRPM3).
In healthy cells the cell receptor transfers calcium from outside the cell to the inside. Here it helps to regulate protein production and gene expression.
In people with CFS calcium isn't getting inside the cells as it should.
This cell receptor is found on every single cell in the body, which would explain the severity of CFS/ME.
It also explains why the illness CFS leads to different symptoms in different people. For example, this dysfunction of cell receptors affects the brain, the spinal cord, and the pancreas.
The research could lead to future CFS treatments and a long hoped for test for CFS.
Hypothesis, subject to further research:
The cause of faulty TRPM3 receptors could explain why many people experience
CFS/ME following a traumatic event or serious infection.
'Threat receptors' such as TRPM3 are upregulated when the body is under any
kind of threat, such as infection, trauma, or even childbirth.
Katherine says: As usual, it is all too complicated for me! But how heartening that it provides a potential explanation for why the illness can follow both infection or trauma and why there are such different Chronic Fatigue Syndrome symptoms in different people.
Click through to this article on sciencealert.com to find out more.
Click here for another page of Chronic Fatigue Syndrome research projects and their findings.
Move to TOP
Click below to move to the home page for www.HealingCFSME.com
- Home Page
- CFS/ME News
Receive daily inspiration...
by putting your favorite (favourite) healing quote on
a mug, cushion, postcard, coaster, T shirt etc.
You will find my zazzle gift store at
zazzle.com/HealingStore.
Use one of my designs or start from a blank.
Thank you from me, Katherine, author of HealingCFSME.com
 |
© Katherine T Owen. All articles on this website are copyrighted. I am delighted if you choose to click above to share this page on social media, but please
do not copy, print or otherwise use without my permission. Thank you. Disclaimer:
I am not a medical practitioner. The articles on this website are not
to be taken as medical advice. Please consult a medical practitioner as
necessary. |